In some cases, untreated Dry Eye Baltimore, MD can lead to pain and permanent vision changes. Doctors evaluate symptoms and design a treatment plan to reduce inflammation, increase tear production, and improve home and work environments.
Self-care tips include adding walnuts and fish to your diet (to boost omega-3 fatty acids) and using a humidifier. They also may recommend prescription eye drops and ointments that lubricate and prevent tear evaporation.
Tears
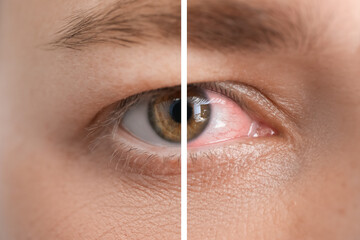
When you blink, a tear film spreads over the eye to keep it healthy and clear. It includes an oily layer (meibum) that prevents tears from evaporating, and a watery middle layer that washes away debris and keeps the eyes hydrated. Dry eye is when the glands in and around your eyes don’t make enough of these tears or they evaporate too quickly, leading to symptoms like itchy or gritty eyes, redness, watery eyes and a feeling that there’s something stuck in your eye.
Several things can cause dry eye, including age-related changes, certain medications (especially antibiotics and antidepressants, heart medicines and diuretics), environmental irritants such as cigarette smoke and systemic diseases such as Sjogren’s syndrome. In addition, prolonged use of computers and other digital devices can reduce natural tear production.
If you have a mild case of dry eye, your doctor may recommend over-the-counter artificial tears. Look for preservative-free drops that come in single-use vials. Also, ask your doctor if adding a humidifier to your room or avoiding irritants such as cigarette smoke can help.
More severe cases of dry eye may require a prescription medication called cyclosporine A or lifitegrast (Restasis or Xildra). These medicines reduce inflammation in your tear glands and increase tear production. They work best when you use them regularly, at least twice a day. You might experience some stinging or irritation when you start the medication, but these symptoms should go away over time.
If over-the-counter treatments don’t improve your symptoms, your doctor can perform a comprehensive eye exam to determine what’s causing them. Your doctor might use a test called the Schirmer tear test, which measures your tear production by placing a strip of paper under your lower eyelid and then counting how many tears it absorbs in five minutes. Your doctor can then prescribe treatment to help manage your symptoms and address the underlying cause of your dry eye. This may include recommending artificial tears, ointments or prescription eye drops. They might also advise you to change your lifestyle, such as taking more breaks from computer screens and limiting irritants in your environment or adding a humidifier to your home or office.
Eyelids
When you blink, your tears spread across the surface of your eye and help lubricate it, reduce your risk for eye infection and wash away dust or debris. Any excess tears flow into small drainage ducts in the inner corners of your eyes and drain into the back of your nose. Dry eye can occur when tear production and drainage are out of balance, as well as due to underlying conditions like contact dermatitis or styes (chalazia).
Whether it’s a new product you’ve slathered on your skin or allergens from perfume droplets, irritants in the air or even just the wind, your body may react negatively to some things and make it flaky around the eyes. “If you are experiencing itchiness or flaking of the skin around your eyes, that can be a sign that there is an underlying condition,” Dr. Libby explains. Some common causes of itchy or flaky eyelid skin include atopic dermatitis, contact dermatitis, seborrheic dermatitis, styes and other conditions that can cause inflammation like psoriasis or eczema.
In addition to anatomical issues, age can also play a role in dry eye symptoms. “As you get older, the natural oils that keep your eyes lubricated decrease, which leaves parts of the eyeball exposed to evaporation,” says Dr. Glass. Moreover, the fats that naturally occur on the eyelid skin are also reduced with aging which can contribute to dryness and irritation.
The other major way your eyelids help lubricate your eyes is by producing some of the complex layers of the tear film, she says. “They produce a mixture of water, mucus, and oil that helps prevent your tears from evaporating too quickly,” she explains.
So if you’re suffering from these signs and symptoms, don’t hesitate to call your eye doctor. Your doctor will be able to diagnose the cause and provide treatment options to help you find relief from dry eye and restore your quality of life. Typically, your doctor will recommend an over-the-counter or prescription topical corticosteroid ointment that works to reduce inflammation, along with other soothing products and techniques for your skin.
Eyesight
Every time you blink, a thin layer of tears spreads across the surface of the cornea, nourishing it and smoothing its texture. But when you have dry eye, that natural process can’t happen as well and your vision suffers. Blurry or gritty eyes are common symptoms of this eye condition, and many patients report having to rub their eyes often to clear their vision.
A growing body of research supports the idea that dry eye negatively impacts not only comfort, but also day-to-day visual function and quality of life. For instance, several studies indicate that dry eye degrades functional visual acuity, meaning that when patients perform sustained visual tasks like reading or staring at digital devices for long periods of time, their ability to concentrate and maintain their clarity decreases.
This is due to a variety of factors, including reduced tear production and increased tear film evaporation. Some medical conditions, such as inflammatory eyelid disorders (blepharitis or rosacea) and certain medications (like antihistamines, NSAIDs, and birth control pills), can also worsen symptoms of dry eye.
Luckily, you can take steps to prevent dry eye symptoms by taking regular breaks from screens, drinking plenty of water and using a humidifier to add moisture to the air. If these home remedies aren’t effective, talk to your ophthalmologist about prescription eye drops to stimulate tear production or decrease inflammation.
When you go in for your dry eye exam, your ophthalmologist will check the thickness of your tear layer and the health of your cornea. They will also examine how you blink, which is an important indicator of your tears’ health.
Your ophthalmologist will likely recommend over-the-counter artificial tears or gels to treat your dry eye symptoms and may refer you for further evaluation if they suspect you have a more severe type of the disease. If you wear contact lenses, they’ll advise you on the best types for your specific type of dry eye.
If you have a serious case of dry eye, your doctor may recommend punctal plugs or other ocular implants to help regulate tear flow and increase the stability of the tear film. They may also recommend dietary changes or supplements to promote eye health, like omega-3 fatty acids.
Treatment
When you have dry eye, treatments include lubricating drops, gels or ointments, over-the-counter or prescription, to help relieve symptoms. You can also try other strategies to reduce symptoms such as using a warm compress on your eyes, washing your hands before touching your eyelids and adding omega-3 oils or fish oil supplements to your diet. Your doctor may recommend that you see an ophthalmologist (eye specialist). Before your appointment, make a list of all your symptoms and how long you’ve had them. Also, list any vitamins, supplements or medicines you take, both prescription and non-prescription.
Your ophthalmologist will examine your eyes and the areas around them, including the eyelids, to diagnose dry eye. They may use special dyes or other tests to check for the condition.
Treatments for dry eye usually focus on reducing inflammation and improving tear production or increasing tear thickness. The first step is to get rid of any infection, which can cause inflammation. Then your ophthalmologist will prescribe medications for the dryness.
A nasal spray called varenicline (Tyrvaya) increases basal tear production by stimulating the trigeminal nerve. It takes a month to start working, but can be effective in relieving dry eye symptoms. Your ophthalmologist might also recommend artificial tears that contain a fatty acid, such as cyclosporine. These are used twice daily in each nostril and can be effective in treating dry eye. Another option is lifitegrast (Xiidra), which is similar to cyclosporine but doesn’t require a prescription and works more quickly.
If your condition is severe, your ophthalmologist may recommend autologous serum drops, which are custom-made artificial tears made from part of your own blood. These can be effective, but they’re expensive and your insurance may not cover them.
Your ophthalmologist might also consider punctal occlusion, in which they close the duct that drains your tears from your lower eyelids (punctum). They’ll put a temporary plug into the punctum to see if it helps. If this is successful, they can insert a permanent plug. Your ophthalmologist might also advise you to avoid certain drugs that can cause dry eye, such as antihistamines, NSAIDs and blood pressure medications.